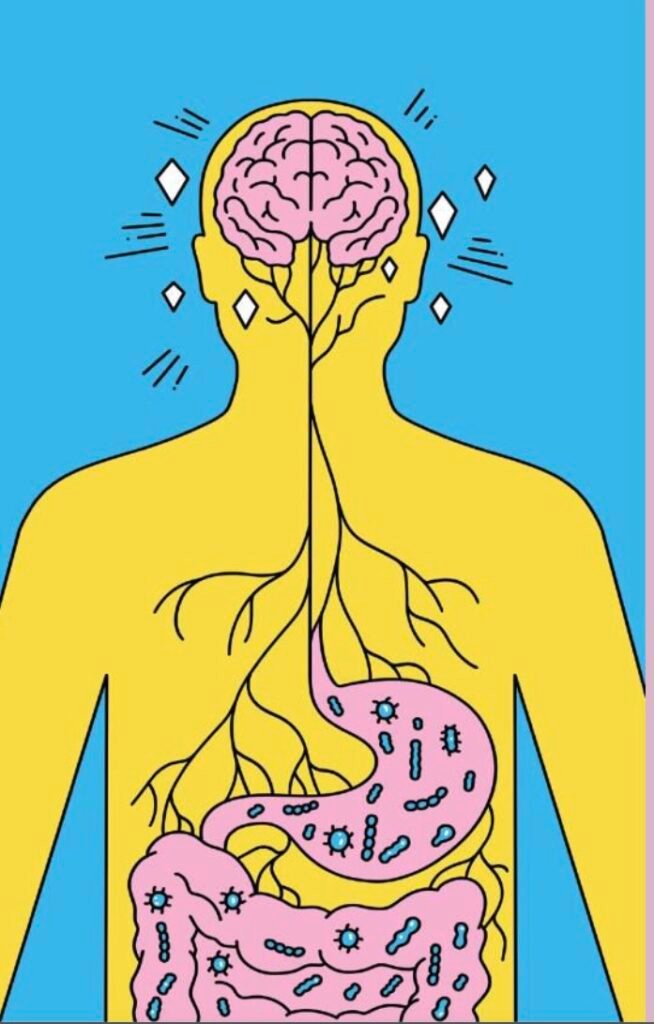
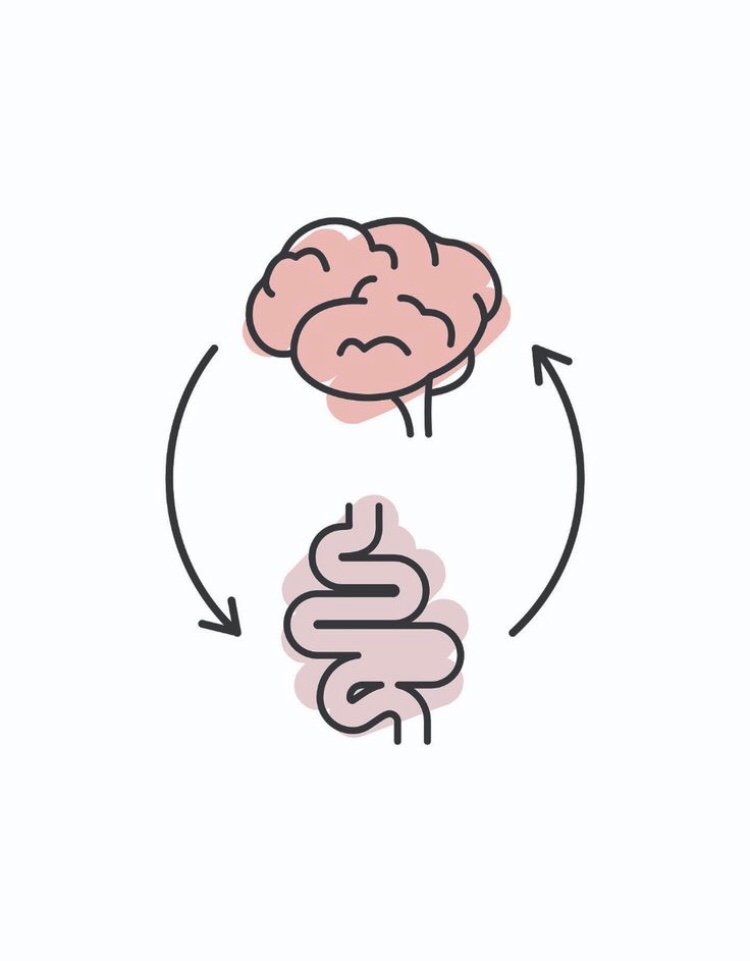
The brain-gut axis, an intricate web of neural, hormonal, and immunological pathways, bridges the gap between our central nervous system (CNS) and the enteric nervous system (ENS). This bi-directional communication profoundly influences both our mental and physical well-being. Recent scientific investigations have illuminated its pivotal role in anxiety management and cognitive function.
At the heart of this connection lies the integration of the CNS and ENS. The vagus nerve, gut microbiota, immune pathways, and neurotransmitters collaborate, allowing seamless communication. This network regulates not only digestion but also mood and cognitive processes, emphasizing the gut’s profound influence on brain health and vice versa.
Anxiety and the Brain-Gut Axis
Neurotransmitter Production: Within our gut, microbiota diligently synthesize neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA). These molecules are essential for mood regulation. An imbalance in gut microbiota—known as dysbiosis—can lead to reduced neurotransmitter production, potentially contributing to anxiety.
Inflammation and Immune Response: Gut inflammation triggers the release of pro-inflammatory cytokines. These cytokines can cross the blood-brain barrier, potentially altering brain function and inducing anxiety.
Vagus Nerve Signaling: The vagus nerve acts as a primary conduit for brain-gut communication. Stress and anxiety can disrupt vagal tone, affecting gut function and exacerbating anxiety symptoms.
Cognitive Function and the Brain-Gut Axis
Neuroplasticity and Neurogenesis: The gut microbiota significantly influences the production of brain-derived neurotrophic factor (BDNF), a protein critical for neuroplasticity and neurogenesis. A healthy gut microbiota enhances cognitive functions such as learning and memory.
Metabolic Byproducts: Short-chain fatty acids (SCFAs), produced during the fermentation of dietary fibers by gut bacteria, exhibit neuroprotective properties. SCFAs modulate gene expression related to cognitive function and synaptic plasticity.
Microbial Metabolites: Specific gut bacteria generate metabolites that can cross the blood-brain barrier, impacting brain function. For instance, tryptophan metabolites can convert into serotonin—a neurotransmitter crucial for cognition and mood regulation.
Therapeutic Implications
Probiotics and Prebiotics: Targeted supplementation with probiotics and prebiotics can restore gut microbiota balance, potentially alleviating anxiety and enhancing cognitive function.
Dietary Interventions: Diets rich in fiber, polyphenols, and omega-3 fatty acids support a healthy gut microbiota, promoting brain health and reducing anxiety.
Psychobiotics: These live organisms, when consumed adequately, confer mental health benefits. Strains like Lactobacillus and Bifidobacterium show promise in anxiety reduction and cognitive improvement.
In conclusion, unraveling the brain-gut axis holds the key to managing anxiety and optimizing cognitive health. By leveraging diet, probiotics, and other interventions, we can potentially alleviate anxiety and enhance mental well-being. However, further research is crucial to uncover precise mechanisms and develop targeted therapies for mental health optimization.





You must be logged in to post a comment.